What risks are we willing to take to (maybe) end malaria?
25.04.22 – After a tremendous decrease in malaria cases in the last two decades, malaria is on the rise again, having killed 677.000 people in 2020, among them 80% children under 5. Apart from being deadly, malaria is detrimental for the livelihoods of entire families, communities and countries: farmers not being able to sow their seeds on time, mothers not being able to sell surpluses on markets to earn a living or children not being able to go to school and benefit from education – a vicious cycle of poverty. While this disease affects one third of the world’s population, some scientists suggest that a new technology called gene drive could be a game-changer.
Gene Drives – manipulating the DNA of mosquitoes to pass down an extinction gene
The research consortium Target Malaria, mostly funded by the Bill & Melinda Gates Foundation and the Open Philanthropy Fund, is developing genetically engineered mosquitoes in the lab that would either make all offspring male or all female offspring infertile. They use the Crispr-Cas methodology to implant a system into their DNA that would replicate when mosquitoes mate, ensuring that this gene spreads throughout the wild mosquito population. But while some hope that this would be the magic bullet to suppress mosquitoe populations and stop the malaria transmission cycle, this currently unproven high risk technology poses fundamental questions for humanity: How far are we willing to go, how high can the risks and uncertainties be in order to test a hypothesis?
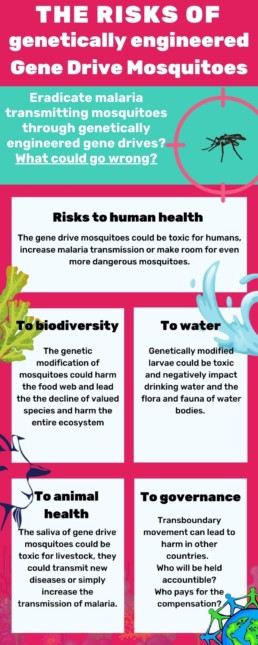
The Risks of Gene Drive mosquitoes
The risks and consequences of genetic engineering are very hard to predict, especially when the organism is supposed to live and mate in the wild. This is because genes do not only affect the physical shape of animals but also their behavior, their interactions with other species and the way bacteria and parasites affect them. A suppression/eradication gene drive is going to have repercussions along the entire food web and would likely mean that their ecological niche will be occupied by another species, and that the plasmodium parasite (which causes malaria) would lack a host – with unknown consequences. In addition, there is a risk that the modified genes could be passed from the mosquitoes via ‘horizontal gene transfer’ to other species and suppress their population too. If this would affect so called “valued species”, the ecosystems could collapse or be severely damaged.
At this point in research scientists do not know if the genes might be toxic for humans or create allergic reactions. Furthermore, the expected change in behavior of the mosquitoes could lead to increased biting and/or even increased malaria transmission. Also, if humans eat animals that ate the gene drive mosquitoes before they could suffer from secondary toxic effects. Last but not least, if the anopheles gambiae mosquito is eradicated, potentially another mosquito could take its spot, increasing the burden of other diseases.
Same as for humans, gene drive mosquitoes could be toxic for livestock, transmit new diseases or may even – counter-intuitively – increase the transmission of malaria.
Mosquito larvae play an important role in water bodies. Genetically modified larvae could be toxic and negatively impact drinking water and the flora and fauna of water bodies.
As this technology is still very new, naturally studies and discussions on their risks, possible adverse consequences as well as the type of global governance and international regulation needed are only in their infancy. For example, guidance materials for risk assessment have not even been commissioned by the global community. In addition – a plethora of important political, socio-economic, cultural and ethical questions remain unaddressed and unanswered. For example, who should be included in the decision making process and who should be consulted before any release? Would it be enough that a national government such as the Burkinabe government allows such a release and that local village chiefs give their consent? How would decision-making processes be designed to uphold the internationally enshrined rights of Indigenous peoples and local communities to say no to projects that could affect them and their territories? Who would be held responsible and who would have to pay for compensation if the gene drive mosquitoes crossed borders and had adverse impacts on ecosystems or farming in non-target environments?
At the same time there are measures at hand that have in the past been used to end malaria in countries such as, most recently, China and El Salvador, being officially declared malaria free in 2021, preceded by Algeria and Argentina in 2019.
What have been the most successful tools to fight malaria?
Research suggests that the number one tool for the decrease of malaria since 2000 are insecticide-treated bed nets. Approximately 65% of the progress achieved between 2000 and 2015 result from the use of these nets.
Poor Water and Sanitation conditions are associated with a number of diseases, among others with the occurrence of malaria. A better sanitation situation would be a holistic approach to fight malaria, while also fighting diarrhea and respiratory infections that kill millions of children every year. Further research shows that good sanitation and piped water are associated with a lower prevalence of malaria among the population. Dr. Sory shares this opinion and believes that correct drainage systems would heavily lower the burden of malaria.
Artemisinin was rediscovered by the Nobel Prize laureate Tu Youyou who found the cure for malaria in traditional books. It is a component from the Artemisia plant. Drugs against Malaria now often contain artemisinin and can cure all malaria strains present nowadays. Initial research suggests that a tea prepared with the Artemisia plant can have preventive and curative effects. It seems that another plant of the Artemisia family, Artemisia afra, could have similar effects, without containing artemisinin. Lucile Cornet-Vernet and Arnaud Nouvion said that more clinical studies are needed to prove once and for all that these plants work. Until now the WHO asks to not use the plant as tea to not cause resistance to artemisinin. Resistances to artemisinin have been discovered in South-East Asia, but not in Africa so far. Lucile Cornet-Vernet on the other hand points to the fact that in China, this plant has been used for about 2000 years and no resistance has been discovered there yet. Furthermore, the plant comes with a variety of components that could potentially cure malaria, thereby being a “poly-therapy”. Access to health care providers diagnosing malaria and prescribing the drug and the financial means to afford them are the limiting factor here. Or else access to seeds or the Artemisia leaves to cure oneself could be useful, if clinical studies can be conducted and no link to the creation of resistance can be drawn.
There is a multitude of repellents that can protect humans between 3-10 hours from mosquito bites. Seen that most mosquitoes bite in the evening/night, this protection is very helpful when going out late. Many of them have chemical ingredients and some have plant-based ingredients. Amongst those, the German society for tropical medicine, travel medicine and global health recommends only the ones with oil from the lemon eucalyptus and points out that for the other natural repellents too little studies have been conducted. This could be a path worth exploring.
Early detection helps people first to get the needed medicine as soon as possible, suffer the least impact of the disease, and second it helps to decrease the risk of a local outbreak in a community.
A new vaccine was recently approved by the WHO for children under 5 years old. A pilot phase was concluded in Ghana, Malawi and Kenya. Employed prior to high transmission periods of malaria this vaccine seems to have positive affects on immunization. It is recommended that children above 5 months get four doses of the vaccine. Over a 4 years follow-up the efficacy of the vaccine against malaria was 36%.
Why is there still malaria in the world then?
To fight malaria the whole toolbox of measures (as mentioned above) needs to be employed, ranging from prevention through nets and repellents, to access to rapid tests to break the infection chain and access to medicine a few hours after being bitten to cure humans. Adding to this; a holistic approach, including urban planning, education, drainage systems and access to health care is needed to fight malaria – as well as many other diseases that trap people in poverty and create a vicious cycle.
What is the Stop Gene Drives Campaign asking for?
In light of the huge variety of to date unassessed possible environmental, health and socio-economic hazards, the potential for economic and political conflict and a plethora of social, ethical and cultural caveats that the environmental use of gene drive technology would entail , the Stop Gene Drive Campaign demands a global moratorium on the release of gene drive organisms. This means that no gene drive organism should be allowed to be released into the environment – not even for field trials – unless a range of conditions have been fulfilled. Read our policy recommendations here.
It seems to us that malaria prevention funds should be directed at strengthening local health care systems, sanitation and education to turn the fight against malaria into an intersectional approach to fight poverty and neglected diseases in general.
__________
Further readings:
Read more about possible gene drive applications here
Read our FAQ about gene drives here
Read more about gene drive regulation here
Read our interviews with experts on malaria prevention here
_________
References:
Connolly, J. B., Mumford, J. D., Fuchs, S., Turner, G., Beech, C., North, A. R., & Burt, A. (2021). Systematic identification of plausible pathways to potential harm via problem formulation for investigational releases of a population suppression gene drive to control the human malaria vector Anopheles gambiae in West Africa. Malaria Journal 2021 20:1, 20(1), 1–69. https://doi.org/10.1186/S12936-021-03674-6
Czechowski, T., Rinaldi, M. A., Famodimu, M. T., Van Veelen, M., Larson, T. R., Winzer, T., … Graham, I. A. (2019). Flavonoid Versus Artemisinin Anti-malarial Activity in Artemisia annua Whole-Leaf Extracts. Frontiers in Plant Science, 10, 984. https://doi.org/10.3389/FPLS.2019.00984/BIBTEX
ENSSER, VDW, & Critical Scientists Switzerland (CSS). (2019). Gene Drives. A report on their science, applications, social aspects, ethics and regulations. Retrieved from https://ensser.org/publications/2019-publications/gene-drives-a-report-on-their-science-applications-social-aspects-ethics-and-regulations/
Guidance on the environmental risk assessment of genetically modified animals. (2013). EFSA Journal, 11(5). https://doi.org/10.2903/J.EFSA.2013.3200
Landier, J., Parker, D. M., Thu, A. M., Carrara, V. I., Lwin, K. M., Bonnington, C. A., … Nosten, F. H. (2016). The role of early detection and treatment in malaria elimination. Malaria Journal, 15(1), 1–8. https://doi.org/10.1186/S12936-016-1399-Y/TABLES/1
Laurens, M. B. (2020). RTS,S/AS01 vaccine (MosquirixTM): an overview. Human Vaccines & Immunotherapeutics, 16(3), 480. https://doi.org/10.1080/21645515.2019.1669415
Malariaprophylaxe und Empfehlungen des Ständigen Ausschusses Reisemedizin (StAR) der DTG. (2021, August). Retrieved April 18, 2022, from https://www.dtg.org/images/Startseite-Download-Box/2021_DTG_Empfehlungen_Malaria.pdf
Maskin, E., Monga, C., Thuilliez, J., & Berthélemy, J. C. (2019). The economics of malaria control in an age of declining aid. Nature Communications 2019 10:1, 10(1), 1–5. https://doi.org/10.1038/s41467-019-09991-4
Okumu, F. O., Govella, N. J., Moore, S. J., Chitnis, N., & Killeen, G. F. (2010). Potential Benefits, Limitations and Target Product-Profiles of Odor-Baited Mosquito Traps for Malaria Control in Africa. PLOS ONE, 5(7), e11573. https://doi.org/10.1371/JOURNAL.PONE.0011573
Prüss-Ustün, A., Wolf, J., Bartram, J., Clasen, T., Cumming, O., Freeman, M. C., … Johnston, R. (2019). Burden of disease from inadequate water, sanitation and hygiene for selected adverse health outcomes: An updated analysis with a focus on low- and middle-income countries. International Journal of Hygiene and Environmental Health, 222(5), 765–777. https://doi.org/10.1016/J.IJHEH.2019.05.004
Q&A on RTS,S malaria vaccine. (n.d.). Retrieved April 18, 2022, from https://www.who.int/news-room/questions-and-answers/item/q-a-on-rts-s-malaria-vaccine
Target Malaria. (n.d.). The Science: What is gene drive? Retrieved from www.targetmalaria.org/ourwork
Target Malaria | Together we can end malaria. (n.d.). Retrieved April 25, 2022, from https://targetmalaria.org/
The Nobel Prize | Women who changed science | Tu Youyou. (n.d.). Retrieved April 19, 2022, from https://www.nobelprize.org/womenwhochangedscience/stories/tu-youyou
WHO. (2019). The use of non-pharmaceutical forms of Artemisia. Retrieved April 19, 2022, from https://www.who.int/news/item/10-10-2019-the-use-of-non-pharmaceutical-forms-of-artemisia
WHO. (2022). Countries and territories certified malaria-free by WHO. Retrieved April 18, 2022, from https://www.who.int/teams/global-malaria-programme/elimination/countries-and-territories-certified-malaria-free-by-who?msclkid=949a737cbf0711ec9474c0ab673942f3
Yang, D., He, Y., Wu, B., Deng, Y., Li, M., Yang, Q., … Liu, Y. (2020). Drinking water and sanitation conditions are associated with the risk of malaria among children under five years old in sub-Saharan Africa: A logistic regression model analysis of national survey data. Journal of Advanced Research, 21, 1–13. https://doi.org/10.1016/J.JARE.2019.09.001
Yasri, S., & Wiwanitkit, V. (2021). Artemisinin resistance: an important emerging clinical problem in tropical medicine. International Journal of Physiology, Pathophysiology and Pharmacology, 13(6), 152. Retrieved from /pmc/articles/PMC8784654/